A Medical billing audit is often thought of as a defensive measure. A government or private payor has denied or pended a series of claims. Now they want to review documentation in the medical records that supports the claims. At that moment, you may be wondering if your documentation meets the guidelines from Medicare or commercial payors. Maybe the thought crosses your mind that you should have had a review of your overall medical billing process after all when your billing manager last suggested it.
In this Article …
- Medical Billing Audit – Offense, not Defense
- The Micro Approach to Billing Audits
- The Macro Approach to Billing Audits
- Assessing Charge Capture and Medical Coding
- The “Billing” in a Medical Billing Audit
- Evaluating Systems to Record Claim Payment
- Denials and Advance Beneficiary Notices
- Auditing Accounts Receivable Management
- Medical Billing Audit as a Planning Tool
- Summary of the Benefits of a Medical Billing Audit
Medical Billing Audit – Offense, not Defense
Organizing and devoting resources to a medical billing audit is a good idea no matter what your motivation. But the audit process can also be an opportunity to increase the profitability of your practice – especially if you think outside the box. Many times, physicians think of such an audit as only including reviewing documentation in the clinical records. That information is then compared to the diagnosis codes and CPT codes, or procedure codes, submitted with the claims. That is certainly an important part of a medical billing audit. And it can show you places where profitability can be increased.
The Micro Approach to Billing Audits
For instance, billing audits focused on medical record documentation can show you where items or services provided to a patient were not recorded as charges. Maybe your documentation of evaluation and management services supports higher-level CPT coding for some visits. Your clinical records documentation may show you are missing documentation of important quality measures.
Payment from Medicare is increasingly dependent on submitting quality measures via claims or to registries. If you are not documenting and submitting quality measures, you may be subject to a penalty. And penalties have increased over time. You can also earn incentive payments for exceptional performance. Medical billing audits can often show that there are easy ways to become an exceptional performer and earn these incentive payments.
Our Revenue Cycle Best Practices Checklist will get you started!
The outcome of this type of medical billing audit – which we will call the “micro” approach – usually results in additional training for physicians and staff. Incomplete staff procedures are strengthened. Physicians and other clinical healthcare providers receive training on improving clinical documentation and exercising proper coding protocol. The quality of patient care and medical records can both improve. This leads to increased payments for the services provided, as well as the potential for incentive payments.
So if this is the “micro” approach, what is the “macro” approach to a medical billing audit?
The Macro Approach to Billing Audits
The macro approach to medical billing audits involves recognizing that the profitability of your medical practice depends on many things. Of course, your effort and skills as a clinician are at the top of the list. However, the amounts you submit on claims and the efficiency of the billing and collections process also affect profitability.
Your Fee Schedule
Many physician practices set up their billing system to bill Medicare at the exact Medicare allowable payment rates. This way, the account balance will be zero after Medicare, the patient and/or a secondary payor makes payment. Anyone using this technique must be sure to keep their billing system up to date each year as the Medicare physician fee schedule changes. Otherwise, Medicare will pay the lesser of the billed charges or the physician fee schedule.
Contracts with Insurance Companies and Health Plans
Contracts with insurance companies and health plans are another area that contributes to profitability. Many insurance companies utilize a fixed fee schedule. The negotiation is “take it or leave it”. But other companies will negotiate fees. Your leverage depends on how important your location or specialty is to their provider network. When you talk to a contracting representative, try to figure out what makes physicians attractive to be included in their network. Services such as after-hours visits or Saturday hours may make a difference, and get you better rates. And attempt to renegotiate every year. Insurance companies are quite willing to pay you the same rates year after year if you never ask for an increase.
Patient Scheduling and Eligibility Verification
We often say that the billing process starts when the patient’s appointment is booked:
Verify the patient’s coverage at this point.
- Counsel patients on their financial responsibilities and the expectation of making copayments at the time of the visit.
- Be sure to put up a sign advising patients of the expectation to make copayments at the time of service.
- Discuss any need for a discount for patients paying cash, or for a hardship discount for patients covered by government programs.
- Be prepared to accept payment in a variety of ways. Cash, credit or debit cards, or checks with instant verification are all forms of payment you should be prepared to accept.
- And don’t forget to remind patients of past-due balances and ask for payment when scheduling future appointments, too.
Many practice management software applications can provide real-time linkage to insurance company eligibility files. Make use of every electronic means available to verify coverage and copayments so the staff stays off the phone with insurance companies.
Physicians vary in the amount of time they want for scheduling various services for patients. It is important in a group practice setting to set some boundaries around scheduling the number of patients and the average length of time allowed for each appointment. Higher patient throughput means overhead is spread over more patients, increasing profitability.
Assessing Charge Capture and Medical Coding
The days of charge sheets and preprinted superbills are pretty much over. Integrated practice management and electronic health records systems can provide for medical coding and capturing charges as part of physician visit documentation. Use these features as much as possible, enabling claims submission within a day or two of service. And don’t forget about capturing out-of-office charges. Hospitalist programs may take the place of primary care physicians making hospital rounds. But there are still many specialties performing procedures in hospitals and surgery centers; capture those charges as soon as possible, too.
The “Billing” in a Medical Billing Audit
What we commonly refer to as billing is more correctly called claims submission. Again, modern practice management systems have enabled the streamlining of the claims preparation process considerably. Electronic clearinghouses accept your claims, scrub them, and submit them to payors. These modern systems have revolutionized the process of preparing and submitting claims. Like any software system, they need maintenance and timely input to realize the maximum benefits of the system. Maintenance includes adding information about new or updated insurance company contracts or payor fee schedules. Timely input includes closing medical records entries soon after visits and capturing out-of-office charges.
Evaluating Systems to Record Claim Payment

Most payors, including Medicare, offer electronic funds transfer as well. This reduces the possibility of embezzlement of payments. Sadly, time and again, a staff member thought to be loyal and dedicated has developed and implemented a scheme to divert physician payments to another account. Remove the temptation and the possibility by signing up for electronic funds transfer whenever possible.
Denials and Advance Beneficiary Notices
Keep track of your denials! Utilize patterns of denials to improve medical documentation. Improved documentation, including appropriate diagnoses that support specific diagnostic or therapeutic procedures, can reduce denials for lack of medical information on the claim.
Other denials may be due to frequency limitations or diagnosis limitations Medicare places on certain diagnostic or therapeutic procedures. When this happens, asking the patient to sign an Advance Beneficiary Notice allows the practice to bill the patient for the service when Medicare issues a denial. Medicare’s requirement for advising the patient on a limitation on the service the physician is recommending can be cumbersome. But better practice management and electronic health record systems enable this process to be completed in a patient-friendly manner.
Auditing Accounts Receivable Management
As the saying goes, you can’t manage what you don’t (or can’t) measure. The best many physician practices manage to do is to track and report the total value of their accounts receivable. Key observations include:
- Tracking only the total value of the AR can result in a lot of issues remaining hidden.
- Maybe your AR is going down because you are not as busy.
- Maybe your AR is steady, but in fact, one payor is paying more quickly while one has slowed down considerably.
- You can improve profitability by reducing your AR, but only if you are collecting more, relatively speaking, of the amounts owed to you.
- An important way to track AR is to measure the days in accounts receivable.
- This is a measure of the average number of days between when you record charges for your services, and the day you collect that revenue.
- To calculate this measure, divide the average daily charges for several months into the total accounts receivable.
How does this help? Well, any number under 30 days would represent very good performance. A number over 60 days would represent opportunities for improvement. Every one-day reduction in Days in AR represents profit for your practice. While this may be a one-time effect, it can be substantial.
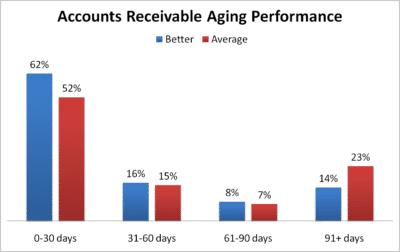
Effective accounts receivable management can improve profitability. The longer it takes to send claims, follow-up on denials and send patient statements, the lower your eventual collections – and profit!
Medical Billing Audit as a Planning Tool
A “macro” level medical billing audit can also serve as a planning tool to keep rightsizing your practice. In-depth analysis can reveal the opportunity to add clinical staff, especially physician extenders like nurse practitioners or physician assistants. These clinicians are very capable, and can easily improve profitability by increasing your patient population while minimizing the increase in overhead.
Summary of the Benefits of a Medical Billing Audit
For most clinicians, the most important part of practicing medicine is serving their patients. But a successful practice also includes running an effective and efficient business. Medical billing audits can go a long way to making yourself successful at both parts of the venture. And this is true of both an internal audit and an external audit.
So let’s wrap up with a brief recap of some of the key takeaways for what medical billing audits cover and provide. And let’s do so separately for each style of audit discussed.
The Benefits that Micro Billing Audits Provide
- Focus on Documentation: The Micro approach primarily revolves around a detailed review of provider documentation. This can show where items or services provided to a patient were not recorded as charges or there was inappropriate coding.
- Quality Measures: Medicare payments are increasingly based on the submission of quality measures. If these measures are not properly documented and submitted, physicians may face penalties. Conversely, documenting and submitting quality measures can earn incentive payments.
- Training and Skill Enhancement: The findings from the Micro approach will usually lead to additional training for medical staff. This includes training on clinical documentation and proper coding protocol.
- Increase in Payments: Improved clinical documentation and proper coding not only help to avoid penalties but can also lead to increased payments and potential for earning incentives.
- Impact on Patient Care: Better documentation can also indirectly lead to better patient care, as the record will be more complete and reflective of the services provided.
So the Micro approach is designed to improve the granularity of clinical documentation and billing at the patient-service level, leading to increased payments and better patient care.
The Benefits that Macro Billing Audits Provide
- Pricing Strategy: Setting a competitive fee schedule and actively negotiating insurance contracts contribute to profitability. Keeping these figures updated and aligned with market standards is crucial.
- Efficient Operations: Streamlining patient scheduling, eligibility verification, and the use of electronic health records can significantly expedite the billing and payment processes, reducing administrative overhead.
- Accounts Receivable Management: Focusing on key metrics like the average number of days to collect revenue can pinpoint areas for improvement and drive profitability.
- Technology Utilization: Employ automated systems for claims submission, payment recording, and other financial transactions to improve efficiency and accuracy, reducing the risk of errors and embezzlement.
- Strategic Planning: Use the macro-level data for long-term planning, including staff expansion and negotiations with payers, to continually adapt and grow the practice in a sustainable manner.
This sums up the Macro approach’s focus on making system-wide changes to improve both profitability and efficiency in a medical practice.


 Verify the patient’s coverage at this point.
Verify the patient’s coverage at this point.
Comments are closed.